Pediatric Brain Cancer AI Prediction Enhances Care Efficiency
In recent years, pediatric brain cancer AI prediction has emerged as a groundbreaking innovation in the fight against childhood cancers, particularly gliomas. By employing advanced AI medical imaging techniques, researchers have achieved significant progress in predicting glioma recurrence, helping to alleviate the stress faced by young patients and their families. This new method leverages temporal learning in medicine to analyze multiple MRI scans over time, providing more accurate assessments compared to traditional prediction methods. Early cancer detection principles are being redefined, paving the way for improved brain tumor treatment strategies that can minimize the frequency of imaging for lower-risk patients. As we delve deeper into this technology, the potential for enhancing care for children battling brain cancer becomes increasingly promising.
The advent of artificial intelligence in the medical field has revolutionized how we approach the diagnosis and management of childhood tumors, particularly in the realm of pediatric brain cancer prognosis. Utilizing innovative AI-driven imaging processes, new methodologies have emerged to predict the likelihood of glioma recurrence with much greater precision than before. This enhanced understanding opens doors for earlier detections of relapse risk, which is crucial for developing tailored interventions. By integrating sophisticated algorithms that employ temporal learning, healthcare professionals can now track subtle changes in patients’ brain scans over time, significantly informing treatment decisions. Consequently, the landscape of brain tumor therapy is shifting towards more informed and patient-centric approaches, ultimately aiming to improve survival rates for children facing these challenging conditions.
Understanding Pediatric Brain Cancer Relapse
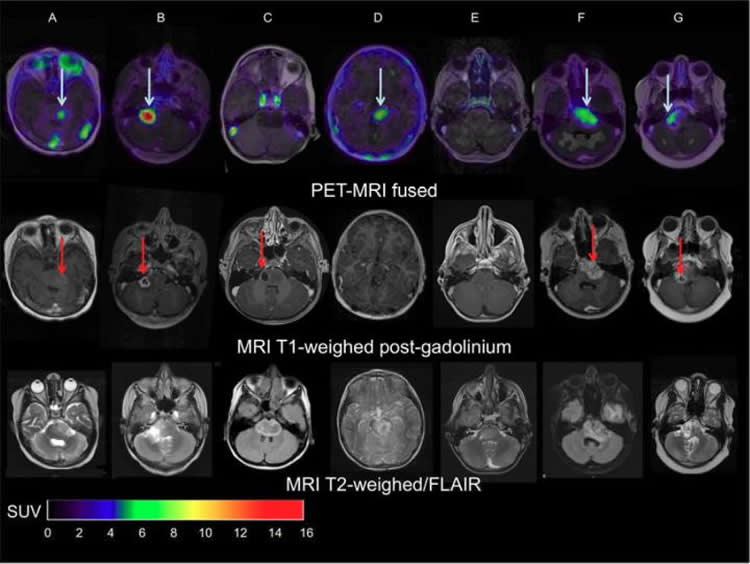
Pediatric brain cancer, particularly gliomas, represents a significant challenge for medical professionals and families alike. These tumors, although often treatable, carry a risk of recurrence that can be devastating for young patients. Early detection of any potential relapse is critical, as it allows for timely interventions that can drastically improve outcomes. Traditional methods of monitoring, which primarily rely on single magnetic resonance imaging (MRI) scans, have shown limitations in accurately predicting when a child might experience a relapse.
Recent advancements in artificial intelligence (AI) have begun to change the landscape of how pediatric brain cancer is monitored. By incorporating AI tools trained to analyze multiple brain scans over time, researchers are identifying patterns that earlier techniques may have missed. This shift not only facilitates earlier intervention but also alleviates some of the emotional and logistical burdens that frequent imaging places on families.
Frequently Asked Questions
How does AI improve pediatric brain cancer diagnosis and treatment?
AI medical imaging enhances pediatric brain cancer treatment by analyzing multiple MRI scans over time, leading to more accurate predictions of glioma recurrence. This allows for personalized follow-up care and reduces the burden of frequent imaging on children and families.
What is the role of AI in predicting glioma recurrence in children?
The AI tool developed for pediatric brain cancer prediction utilizes temporal learning to analyze sequential brain scans. This method significantly improves the accuracy of glioma recurrence prediction, ranging from 75-89%, compared to traditional methods which have a 50% accuracy.
What are the benefits of early cancer detection in pediatric patients using AI?
Early cancer detection using AI can identify high-risk pediatric brain cancer patients sooner, allowing for timely intervention or tailored treatment options. This proactive approach enhances the overall care experience for children with brain tumors.
What techniques does AI use to analyze brain scans in pediatric brain cancer cases?
AI employs temporal learning to sequentially analyze MRI scans from pediatric brain cancer patients, enabling it to recognize subtle changes over time that might indicate a risk of glioma recurrence, improving diagnostic accuracy.
Why is temporal learning important in AI predictions for pediatric brain cancer?
Temporal learning is crucial because it allows AI to synthesize findings from multiple MRI scans taken over time. This approach enhances the predictive capability for glioma recurrence compared to analyzing single images, leading to better patient management.
Can AI methods reduce the need for frequent imaging in children treated for brain tumors?
Yes, AI methods can facilitate more personalized care by identifying low-risk pediatric patients who may not require frequent imaging, thereby alleviating stress on families and patients.
What future steps are researchers considering for AI in pediatric brain cancer treatment?
Researchers plan to conduct clinical trials to validate AI-informed risk predictions for children with brain tumors, aiming to improve treatment protocols and outcomes based on individual patient risk levels.
| Key Aspect | Details |
|---|---|
| AI Tool Efficiency | AI predicts relapse risk with 75-89% accuracy vs. 50% for traditional methods. |
| Temporal Learning | A technique that trains AI on multiple MRI scans over time for better predictions. |
| Study’s Objective | To improve care for children with gliomas by predicting who is at highest risk of recurrence. |
| Research Collaborators | Mass General Brigham, Boston Children’s Hospital, Dana-Farber. |
| Study Findings | Prediction accuracy improves with multiple scans, plateauing after 4-6 images. |
| Future Plans | Further validation and clinical trials are needed for practical applications. |
Summary
Pediatric brain cancer AI prediction has shown significant promise, with a new AI tool demonstrating a higher accuracy in predicting the risk of relapse in pediatric patients with gliomas. Traditional methods have struggled, achieving only 50% accuracy when predicting recurrence, while this advanced approach leverages temporal learning to achieve 75-89% accuracy by analyzing multiple MRI scans over time. This innovative method aims to alleviate the burden of frequent imaging in children, identifying high-risk patients more effectively and potentially leading to improved treatment strategies. Ultimately, ongoing research and clinical trials will further refine these predictions and enhance the care provided to affected children.