CRISPR Gene Editing Ethics: Weighing the Promise and Peril
The ethics of CRISPR gene editing has become a pivotal topic in contemporary discussions of medical innovation and health equity. As scientists harness the power of gene editing technology to potentially cure genetic disorders like sickle cell anemia, profound ethical questions arise regarding the implications of such decisions. Do we possess the moral authority to alter human genetics, especially when contemplating changes that could affect future generations? This dialogue was recently exemplified by notable experts who emphasized that while CRISPR presents remarkable opportunities, it also poses risks that must be critically examined. Addressing these ethical complexities is vital as we navigate the future of genetic engineering and its role in society.
The moral implications surrounding CRISPR’s cutting-edge genetic modification techniques are prompting a reevaluation of our responsibilities within health care. As researchers delve into the realm of genome editing, they unveil the potential to eradicate hereditary diseases such as sickle cell disease, igniting debates on what constitutes acceptable medical practice. The intersection of genetics, ethics, and societal values raises crucial questions about the nature of human variation and the decisions surrounding our genetic futures. By exploring alternative perspectives on gene manipulation, stakeholders are pressed to consider how medical breakthroughs can be aligned with fairness and equity in healthcare. The conversation is no longer just about what can be achieved through technology but also what should be allowed.
Exploring the Ethics of Gene Editing
The advent of CRISPR technology marks a significant turning point in the realm of gene editing, raising essential questions about the ethical implications of manipulating human genetics. As discussed by Neal Baer during his talk, the power to edit the human genome presents a dual-edged sword; while it introduces revolutionary methods for addressing genetic diseases like sickle cell anemia, it simultaneously casts a shadow of moral uncertainty over what constitutes ethical practice in medicine. The ethical debate surrounding CRISPR gene editing is profound, as it challenges our understanding of what it means to be human and how far we should go in altering human conditions.
The concept of ‘playing God’ often arises in these discussions, prompting debates about who gets to decide which traits are preferable and which conditions warrant intervention. As Baer points out, decisions about gene editing could easily be influenced by societal biases, leading to a potential increase in health disparities. The conversation surrounding ethics in gene editing is not just about capability, but also about responsibility, invoking essential discussions about the societal implications of creating inequities in medical innovations.
Health Equity and Access to Gene Therapies
A recurring theme in discussions about sickle cell anemia and CRISPR technology is the concern for health equity. Baer raises critical questions about the costs associated with gene therapies, which can reach upward of $2.2 million. This incredible expense poses a barrier, raising essential questions about who can access these life-altering treatments. For many families, such costs are beyond reach, potentially exacerbating existing health disparities between economically disadvantaged groups and those with greater financial resources. As advancements are made in gene editing, it is vital to address how these innovations can be made accessible to all, particularly marginalized communities that may suffer disproportionately from genetic disorders.
Moreover, the discourse should extend beyond just access to innovative treatments. A comprehensive approach to health equity considers factors such as education, socioeconomic status, and cultural perceptions of gene editing. Medical innovations must not only be available but also comprehensible to all potential beneficiaries. Bridging this gap ensures that advancements in gene therapies serve a broad spectrum of society, fostering an equitable healthcare landscape rather than widening the existing chasm.
The Potential Risks of Genetic Manipulation
While CRISPR presents transformative potential for treating genetic diseases, it also harbors numerous risks that users must carefully consider. There is a significant concern regarding unintended consequences that may arise from gene editing, particularly when it comes to complex traits influenced by multiple genes. For instance, Baer reflects on the advances made by geneticists, like the editing of the gene responsible for controlling LDL cholesterol levels. While lowering cholesterol sounds beneficial, such manipulations could inadvertently interfere with various body processes, highlighting the intricate and interconnected nature of genetics.
Moreover, as discussed by Baer and Brendel, the oversight of gene editing practices remains a significant challenge. With rogue scientists potentially conducting unethical experiments outside of regulatory reach, the consequences of unsupervised genetic manipulation could manifest in ways that are harmful, not just to individuals but to society as a whole. Thus, proper regulations and monitoring are imperative to ensure that CRISPR can be used safely and ethically, guarding against the unintended repercussions that may arise from its misuse.
The Role of Society in Genetic Decision-Making
The discourse surrounding CRISPR gene editing often brings to light the role of societal norms and values in shaping the decisions surrounding genetic modifications. Baer’s articulation of the ethical dilemmas, such as whether two deaf parents should have the right to choose hearing for their child, showcases the delicate balance between parental autonomy and societal implications. This raises broader questions: Should societal consensus establish limits on genetic editing, or should autonomy reign supreme? Such considerations reflect the complexity of human variation and the societal constructs surrounding disability and normalcy.
Moreover, the nuances of genetic decision-making underscore the importance of public engagement in discussions about gene editing. Open forums encompassing diverse perspectives can shed light on community values and ethics, which in turn could guide responsible practices in genetic research. By fostering collaborative dialogues among scientists, ethicists, and the public, society can cultivate a framework where gene editing aligns with collective ethical standards, thus ensuring advancements accompany a robust moral compass.
Navigating Parental Rights and Genetic Choices
A significant aspect of the ongoing debate regarding gene editing involves navigating parental rights when it comes to making decisions about their children’s genetic attributes. As Baer highlighted, some parents may seek genetic modifications to
Frequently Asked Questions
What are the primary ethical concerns regarding CRISPR gene editing?
The ethical concerns surrounding CRISPR gene editing include the potential for unintended consequences of genetic alterations, the moral implications of editing germline cells, issues of consent—especially in the case of future generations—and the risk of exacerbating health inequities. As gene editing advances, society must grapple with the responsibility and authority over decisions that could affect human diversity and individual identities.
How does CRISPR technology impact health equity in gene editing?
CRISPR technology presents significant implications for health equity, particularly in terms of accessibility and affordability. While gene editing offers potential cures for conditions like sickle cell anemia, the high cost—approximately $2.2 million for some treatments—raises questions about who can afford these innovations. This disparity may widen the gap between those who can access advanced medical treatments and those who cannot, thus leading to increased health inequity.
Should we use CRISPR gene editing for non-lethal conditions?
The ethics of using CRISPR gene editing for non-lethal conditions, such as Down syndrome, is contentious. Many argue that altering genes for conditions that do not significantly impair quality of life raises moral questions about societal values and parental autonomy. It challenges us to consider who decides which traits are desirable and the broader implications of ‘designing’ children, emphasizing the need for robust ethical frameworks in gene editing.
What role does consent play in CRISPR gene editing ethics?
Consent is a foundational ethical principle in CRISPR gene editing, particularly concerning germline editing where changes are passed on to future generations. Questions arise about how to obtain informed consent from individuals who cannot yet express their wishes, such as embryos or future children. This highlights the need for ethical guidelines that protect the rights of individuals affected by genetic modifications without their explicit consent.
What are potential risks associated with CRISPR gene editing technology?
Potential risks of CRISPR gene editing technology include unintended genetic consequences, such as off-target mutations and unanticipated interactions of edited genes with other biological systems. This complexity can lead to unforeseen health issues, complicating the ethical landscape of gene editing. Additionally, the possibility of misuse in non-therapeutic contexts—like enhancing physical or mental attributes—raises profound ethical questions about the future of human variation.
How can ethical oversight be ensured in CRISPR gene editing research and applications?
Ensuring ethical oversight in CRISPR gene editing involves developing comprehensive regulatory frameworks that govern research and clinical applications. This includes establishing ethical review boards, regulatory agencies, and international collaborations to monitor CRISPR use. Transparency and public engagement are crucial to foster trust and accountability in gene editing, helping to mitigate potential misuse and ethical violations.
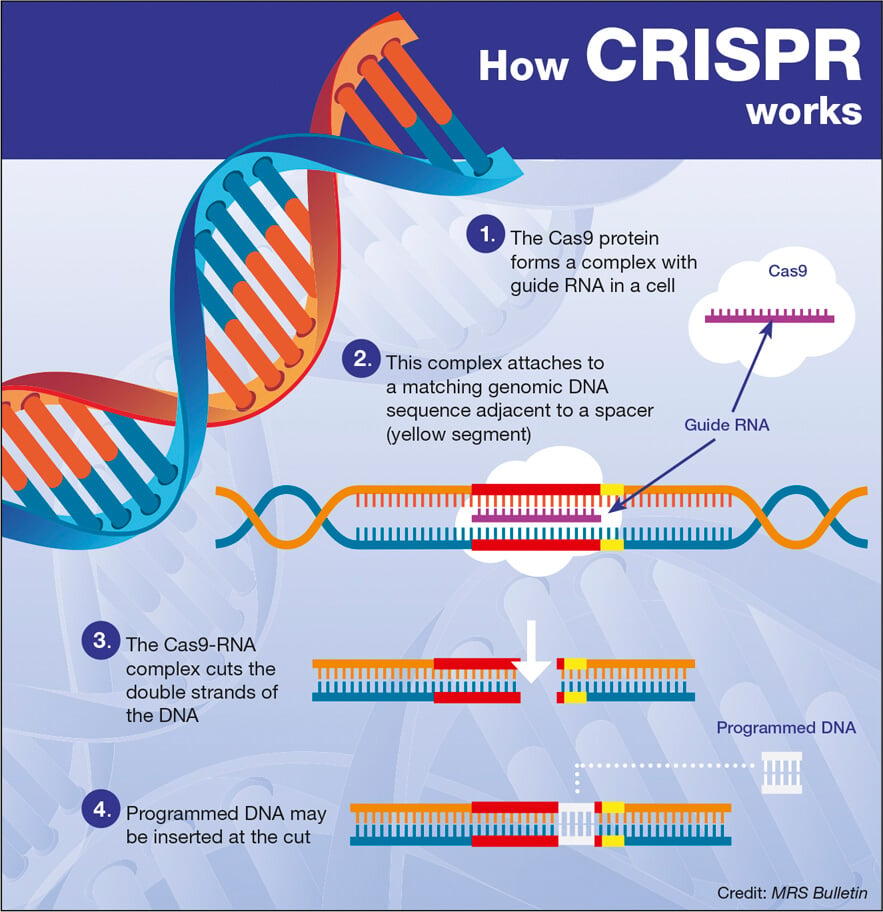
What is the connection between CRISPR gene editing and medical innovation?
CRISPR gene editing represents a groundbreaking advancement in medical innovation, offering the potential to cure genetic diseases and improve health outcomes. However, it also brings ethical challenges that must be addressed to harness its benefits responsibly. Balancing the drive for innovation with ethical considerations underscores the necessity for dialogues about the implications of manipulating human genetics.
What does health justice mean in the context of CRISPR gene editing?
Health justice in the context of CRISPR gene editing involves advocating for equitable access to genetic technologies across all social groups. As gene editing progresses, it is essential to address disparities in healthcare access to ensure that advancements like CRISPR benefit marginalized communities rather than exacerbate existing inequalities. This requires integrated policies that prioritize vulnerable populations in medical innovation efforts.
| Key Points | Details |
|---|---|
| Introduction to CRISPR | Discusses the promise and peril of CRISPR gene editing. |
| Ethical Dilemmas | Questions whether we should change human differences; raises concerns about editing genes for traits associated with life. |
| High Costs | The cost of gene manipulation (e.g., $2.2 million cure for sickle cell) raises issues of accessibility and fairness. |
| Health Equity | The advancements can exacerbate inequalities between those who can afford treatments and those who cannot. |
| Parental Decisions | Questions about parental rights to modify children’s inherent traits. |
| Legal and Oversight Issues | Concerns over lack of regulation in countries like Russia and China regarding genetic modification. |
| Unintended Consequences | Gene editing can have unpredictable effects, complicating the notion of “curing” diseases. |
Summary
CRISPR gene editing ethics are a rapidly evolving field that poses significant moral questions about our ability to alter human genetics. As advancements in CRISPR technology unlock potential cures for severe ailments like sickle cell anemia, we must grapple with the ethical implications of such interventions. The discussions led by experts highlight concerns about equity, the role of parents in making genetic choices, and the governance of gene editing practices globally. Ultimately, while CRISPR presents exciting opportunities, its application necessitates a careful balancing of medical progress and ethical responsibility.