Alzheimer’s Disease Research: Revolutionizing Treatment Approaches
Alzheimer’s disease research has taken a transformative turn, especially through the groundbreaking work of scientists like Beth Stevens, who emphasizes the role of microglial cells in the brain’s immune system. These unique cells not only patrol for signs of illness or injury but are also pivotal in synaptic pruning, a crucial process for neuronal communication. However, when this process goes awry, it can contribute to the development of neurodegenerative diseases, including Alzheimer’s. By understanding the functioning and malfunctioning of microglia, researchers are uncovering new avenues for Alzheimer’s treatment, paving the way for innovative biomarkers and therapies. As the number of Americans affected by Alzheimer’s continues to rise, such research efforts could prove vital in changing the narrative of this incurable disease.
The study of Alzheimer’s disease, often seen as a leading cause of cognitive decline in older adults, is evolving with fresh insights into the brain’s cellular mechanisms. Researchers are increasingly focusing on the immune functions of microglial cells, which play a significant role in maintaining brain health and executing processes like synaptic pruning. Understanding these mechanisms provides hope for potential therapeutic options to combat the effects of various neurodegenerative disorders. Furthermore, as scientists delve deeper into the complexities of the brain’s immune system, they uncover the intricate connections that could lead to groundbreaking Alzheimer’s interventions. This exploration into brain health not only addresses a pressing public health issue but also represents a broader understanding of how our bodies forge resilience against progressive cognitive diseases.
Understanding the Role of Microglial Cells in Neurodegenerative Diseases
Microglial cells are essential to the brain’s immune system, acting as the first line of defense against neurodegenerative diseases such as Alzheimer’s and Huntington’s disease. They constantly monitor the brain environment, identifying harmful agents and promoting the removal of dead cells. This action is vital for maintaining neuronal health, as it prevents the accumulation of debris that could lead to inflammation and further neuronal damage. When functioning correctly, microglial cells support synaptic pruning—a necessary process for normal brain development and function. However, when their activities become unregulated, they can contribute to the very diseases they aim to protect against, highlighting the complexity of brain immunology and its implications for Alzheimer’s treatment.
Research led by Beth Stevens has brought to light how aberrant microglial activity can disrupt normal synaptic pruning processes. In cases of Alzheimer’s disease, microglia can overly prune synapses, leading to cognitive decline and memory loss in affected individuals. This paradoxical behavior underscores the importance of understanding how microglial cells interact with neurons and their environment. Ongoing studies are focused on identifying specific biomarkers that could indicate when microglial cells are functioning improperly, which could pave the way for targeted therapies in Alzheimer’s treatment and other neurodegenerative disorders.
The Impact of Synaptic Pruning on Brain Health
Synaptic pruning is a crucial physiological process that allows the brain to eliminate excess synapses that are no longer needed, thus refining its neural circuits. This process is particularly active during development but continues throughout an individual’s life to facilitate learning and memory. However, improper synaptic pruning can lead to cognitive dysfunction and has been implicated in a variety of neurodegenerative diseases, including Alzheimer’s disease. Understanding how synaptic pruning is regulated by microglial cells could offer insights into how to maintain brain health and prevent conditions associated with neurodegeneration.
In Alzheimer’s disease, the mismanagement of synaptic pruning has been linked to the loss of synaptic connections and neuronal death, contributing to the overall decline of cognitive functions. The Stevens Lab’s research emphasizes the dual role of microglial cells; while they are necessary for synaptic maintenance, their dysregulation can lead to detrimental outcomes. Therapies that aim to restore proper synaptic pruning activity could have a significant impact on preserving cognition in aging populations and those at risk for Alzheimer’s. Ongoing investigations into the interplay between microglial activity and synaptic health remain paramount for future advancements in Alzheimer’s treatment.
How Alzheimer’s Disease Research is Transforming Brain Science
Alzheimer’s disease research has transformed our understanding of the brain’s immune system and its involvement in neurodegenerative conditions. Scientists like Beth Stevens have pioneered work that highlights the role of microglial cells in both maintaining neuronal health and potentially contributing to Alzheimer’s pathology. The insights gained from this research are starting to change the way we view the onset and progression of neurodegenerative diseases, suggesting that targeting the immune response in the brain may be a viable strategy for treatment.
With advancements in biomarker identification and understanding the relationship between microglial cells and synaptic pruning, researchers are beginning to develop new therapeutic approaches to slow or halt the progression of Alzheimer’s disease. The integration of basic science into clinical applications is essential; as we explore how brain immune function affects synaptic health, we can formulate treatments that address the root causes of disease. This evolving field is indicative of a future where Alzheimer’s treatment could rely not only on traditional methodologies but also on innovative strategies derived from cellular-level insights.
The Connection Between Microglial Dysfunction and Alzheimer’s Treatment
Dysfunction in microglial cells has been closely linked to impairments seen in Alzheimer’s disease. These immune cells play a critical role in the homeostasis of synaptic pruning, and when their function is compromised, it may result in inappropriate synaptic elimination and subsequent cognitive decline. This relationship underscores the need for Alzheimer’s treatment approaches that focus on restoring microglial function rather than solely targeting amyloid plaques or tau tangles traditionally associated with the disease. Understanding the mechanisms that underpin microglial behavior could lead to groundbreaking therapeutic strategies that reshape the landscape of Alzheimer’s treatment.
Innovations in Alzheimer’s treatment are increasingly focusing on modulating the activity of microglial cells. By restoring their normal function, researchers aim to reduce synaptic loss and support cognitive functions in affected individuals. Targeted therapies that activate or inhibit specific microglial pathways hold great promise in mitigating the progression of Alzheimer’s disease and enhancing the overall quality of life for patients. A comprehensive understanding of microglial pathology will be critical in developing these novel therapies, translating scientific insights into real-world applications.
The Role of Federal Funding in Advancing Alzheimer’s Disease Research
Federal funding has played a pivotal role in advancing Alzheimer’s disease research, particularly in supporting groundbreaking studies focused on microglial cells and their implications for neurodegenerative diseases. Researchers like Beth Stevens have relied on grants from the National Institutes of Health (NIH) to explore the complexities of the brain’s immune system, which has led to significant discoveries regarding synaptic pruning and microglial dysfunction. This financial support is crucial for fostering innovation and enabling scientists to pursue curiosity-driven research that may eventually lead to viable treatments for Alzheimer’s.
Moreover, sustained investment in Alzheimer’s research through federal funding not only facilitates the exploration of basic science but also fosters collaboration across various disciplines. The intersection of insights from molecular biology, neuroimmunology, and clinical studies strengthens the overall understanding of Alzheimer’s disease. Consequently, as new findings emerge from federally funded projects, the potential for translating these discoveries into effective Alzheimer’s treatments increases, providing hope for millions impacted by this challenging disorder.
The Promise of Biomarkers in Detecting Alzheimer’s Disease
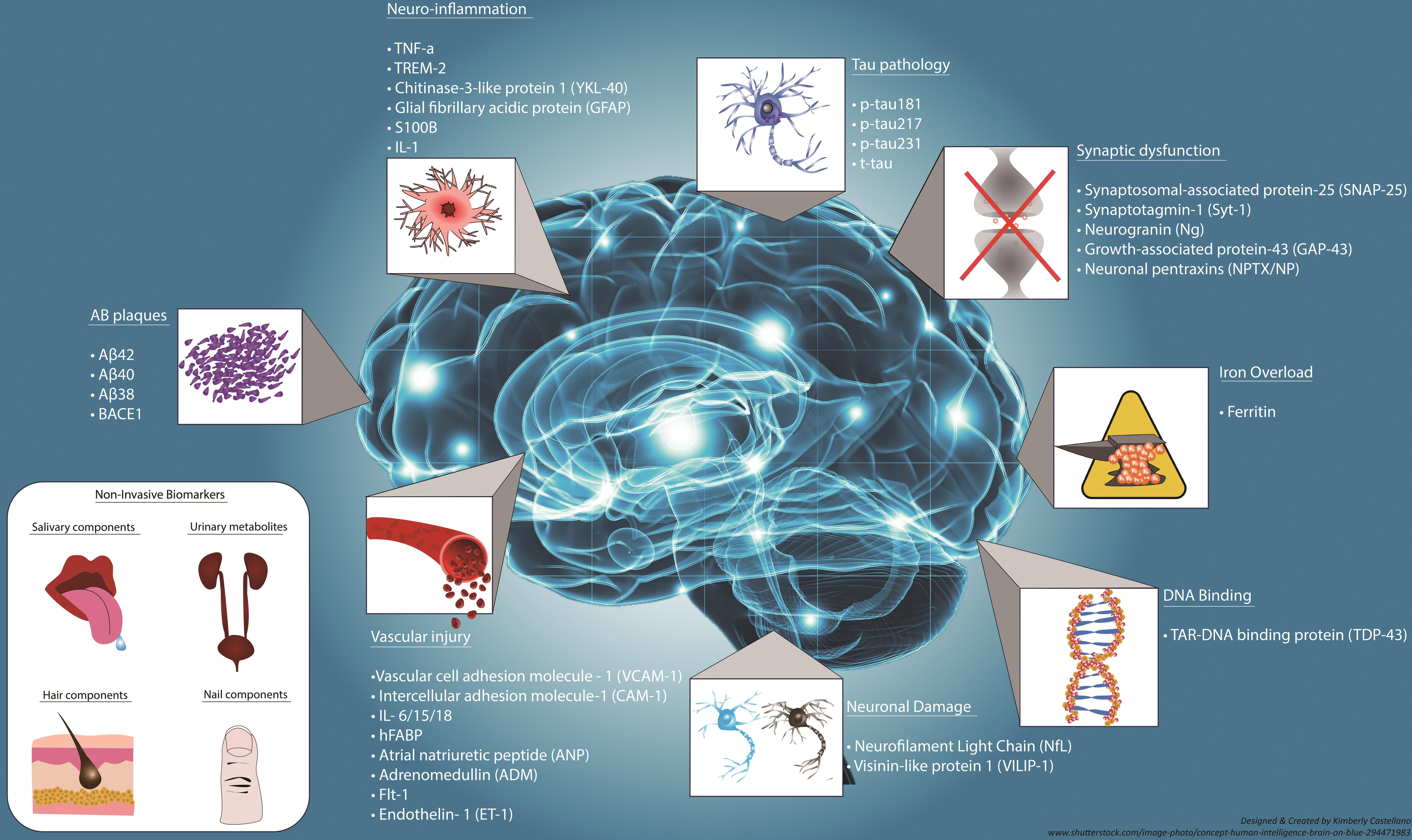
Biomarkers hold great promise for the early detection and monitoring of Alzheimer’s disease, offering a window into the disease’s progression before significant symptoms manifest. Current research efforts are focusing on identifying specific biological markers related to microglial cell activity and synaptic health. With the insights gained from understanding the role of microglial cells in neurodegenerative diseases, scientists aspire to develop reliable biomarkers that can signal when microglia are functioning improperly, leading to earlier intervention and targeted Alzheimer’s treatment.
The implementation of biomarkers in clinical settings may revolutionize how Alzheimer’s disease is diagnosed and managed. By providing quantitative measures of disease progression and immune status, biomarkers can facilitate personalized treatment strategies, allowing clinicians to tailor interventions based on the specific needs of patients. As research continues to unfold, the integration of biomarker testing into standard Alzheimer’s screening could significantly enhance our ability to combat this debilitating disease at its onset.
Innovative Therapies Targeting the Brain’s Immune System
Innovative therapies targeting the brain’s immune system represent a new frontier in Alzheimer’s treatment. Research has shown that modulating the activity of microglial cells can potentially protect neurons from degeneration and restore cognitive function. Interventions designed to enhance microglial support during synaptic pruning are being explored as potential treatment pathways. This approach is particularly promising given the increasing understanding of the intricate relationship between immune function and neurodegenerative diseases.
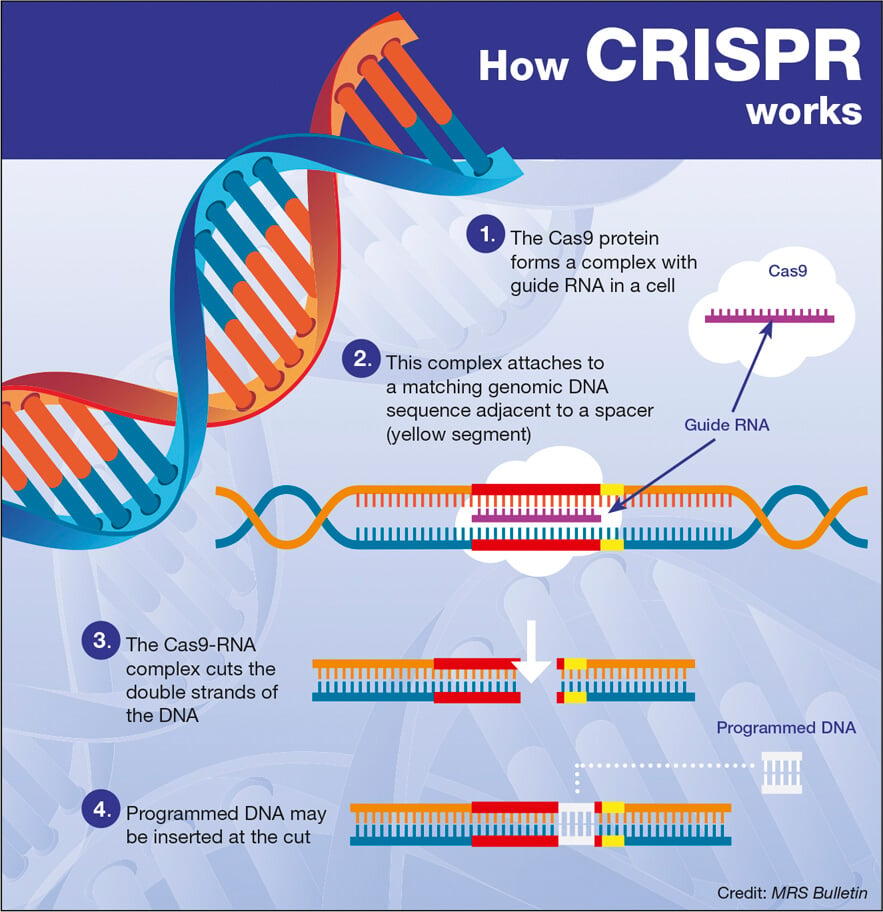
Emerging treatments, including small molecules that influence microglial activation or gene therapies that target specific pathways involved in synaptic maintenance, are at the forefront of Alzheimer’s research. These novel strategies aim to correct the imbalances in microglial cell activity that often accompany neurodegeneration. As future clinical trials evaluate the safety and efficacy of these therapies, there is hope that they can transform the landscape of Alzheimer’s treatment, leading to better outcomes for those affected by this challenging disease.
Curiosity-Driven Research as a Foundation for Alzheimer’s Discoveries
Curiosity-driven research has been a cornerstone of scientific discovery, particularly in the field of Alzheimer’s disease. Researchers like Beth Stevens exemplify how fundamental investigations into microglial cells and their roles in neurodegeneration can lead to significant breakthroughs in understanding disease mechanisms. This type of research allows for the exploration of unexpected avenues that can yield new insights, ultimately benefiting the broader fight against Alzheimer’s and other neurodegenerative diseases.
Emphasizing the importance of basic science, Stevens notes that foundational research done over decades has paved the way for present-day discoveries. The exploration of microglial function and its implications for synaptic pruning underscores the value of curiosity in scientific inquiry. These investigations encourage future generations of scientists to pursue questions that may initially seem tangential but can illuminate critical aspects of disease pathology and therapy development. By fostering an environment where curiosity thrives, the potential for significant advancements in Alzheimer’s treatment becomes increasingly attainable.
Frequently Asked Questions
How do microglial cells relate to Alzheimer’s disease research?
Microglial cells are crucial components of the brain’s immune system and play a significant role in Alzheimer’s disease research. They patrol the brain, clearing dead or damaged cells, and are involved in synaptic pruning—removing unnecessary neural connections. Research shows that aberrant pruning by microglia can contribute to the progression of Alzheimer’s disease, making them a target for potential treatments.
What is the significance of synaptic pruning in Alzheimer’s treatment?
Synaptic pruning is essential in maintaining healthy brain function by eliminating excess neural connections. In Alzheimer’s disease research, it has been found that improper synaptic pruning can lead to neurodegenerative changes. Understanding these processes may lead to new Alzheimer’s treatment strategies that target microglial function, helping to restore healthy synaptic connections and improve cognitive function.
How does the brain’s immune system interact with neurodegenerative diseases like Alzheimer’s?
The brain’s immune system, primarily composed of microglial cells, plays a protective role against neurodegenerative diseases such as Alzheimer’s. These cells actively monitor and respond to brain injuries and infections. Research in Alzheimer’s disease emphasizes how dysfunction in microglial cells and their pruning activity can exacerbate disease progression, highlighting the importance of the brain’s immune system in managing neurodegeneration.
What role do microglial cells play in neurodegenerative diseases other than Alzheimer’s?
Microglial cells are involved in various neurodegenerative diseases beyond Alzheimer’s, including Huntington’s disease. Their function in clearing debris and regulating synaptic pruning is critical in maintaining brain health. Abnormalities in microglial activity can lead to detrimental effects on neuronal connections, contributing to the pathology of multiple neurodegenerative conditions.
Can research on microglial cells lead to breakthroughs in Alzheimer’s disease treatment?
Yes, ongoing research on microglial cells offers significant promise for breakthroughs in Alzheimer’s disease treatment. By understanding their role in synaptic pruning and the brain’s immune response, researchers are working to develop new biomarkers and therapeutic strategies that could potentially slow down or reverse the effects of Alzheimer’s and improve patient outcomes.
What advancements have been made in Alzheimer’s disease research concerning the brain’s immune system?
Recent advancements in Alzheimer’s disease research have focused on the role of the brain’s immune system, especially microglial cells. Studies indicate that microglial dysfunction and improper synaptic pruning can lead to neurodegeneration. This understanding is paving the way for innovative therapies aimed at modulating microglial activity to protect against Alzheimer’s-related damage.
| Key Point | Detail |
|---|---|
| Research Focus | Microglial cells’ role in Alzheimer’s disease and other disorders. |
| Research Implications | Aberrant pruning by microglia can contribute to Alzheimer’s and Huntington’s diseases. |
| Funding Importance | Vital federal support from NIH allowed for the progression of the research. |
| Potential Impact | Research can lead to new biomarkers and medicines to treat neurodegenerative diseases. |
| Future of Research | Basic science underpins applied research leading to better human health outcomes. |
Summary
Alzheimer’s disease research has proven to be a crucial area of study, particularly with the advancements made by Beth Stevens and her team. Their pioneering work on microglial cells highlights the vital role these immune cells play in maintaining brain health and their implications in diseases like Alzheimer’s. By understanding how these cells function, researchers are not only uncovering the pathogenesis behind neurodegenerative disorders but are also paving the way for innovative treatments that could significantly improve the lives of millions affected by Alzheimer’s.