Alzheimer’s Research: Transforming Treatments and Discoveries
Alzheimer’s research represents a pivotal frontier in understanding and combating one of the most pressing neurodegenerative diseases in today’s world. With millions of individuals affected by Alzheimer’s, scientists increasingly investigate the role of microglial cells, the brain’s immune system, in disease progression. These specialized cells are crucial in maintaining brain health, yet their malfunctioning can lead to harmful pruning of synapses, exacerbating memory loss and cognitive decline. Recent breakthroughs in detecting biomarkers for Alzheimer’s have illuminated pathways toward innovative Alzheimer’s treatments that could transform patient care. As we strive to unravel the complexities of Alzheimer’s, ongoing research promises not only hope for those affected but also a clearer understanding of the cellular mechanisms at play in neurodegenerative disorders.
Studies surrounding dementia-related illnesses, particularly those associated with memory loss, highlight the urgency of ongoing exploration in this vital health sector. Groundbreaking insights into the functions of glial cells, which act as pivotal components of the brain’s immune response, are reshaping our perception of neurological health. By examining how these cells interact and their potential implications for conditions such as Alzheimer’s, researchers are uncovering critical clues that could herald new therapeutic avenues. Additionally, the discovery of early-stage biomarkers for neurodegenerative conditions may prove instrumental in diagnosing and intervening before severe degeneration occurs. As we delve deeper into the neural architecture and the immune landscape of the brain, the quest for effective treatments marches on.
The Role of Microglial Cells in Alzheimer’s Research
Microglial cells play a crucial role in the brain’s immune system, acting as the first line of defense against neurodegenerative diseases like Alzheimer’s. These cells constantly patrol the brain, seeking out cellular debris, damaged neurons, and signs of disease. While their primary function is to maintain brain health, an imbalance in their activity can contribute to the pathogenesis of Alzheimer’s. Research by Beth Stevens has unveiled the implications of microglial cell behavior, revealing that abnormal pruning of synapses can exacerbate the development of Alzheimer’s and other related disorders.
Understanding how microglial cells function not only helps in deciphering the mechanisms behind Alzheimer’s but also opens up potential therapeutic avenues. By targeting the pathways and signaling mechanisms involved in microglial activity, researchers can develop strategies to enhance their protective functions. Moreover, identifying biomarkers associated with microglial dysfunction may facilitate earlier diagnosis of Alzheimer’s, significantly impacting treatment outcomes and quality of life for millions affected by this debilitating condition.
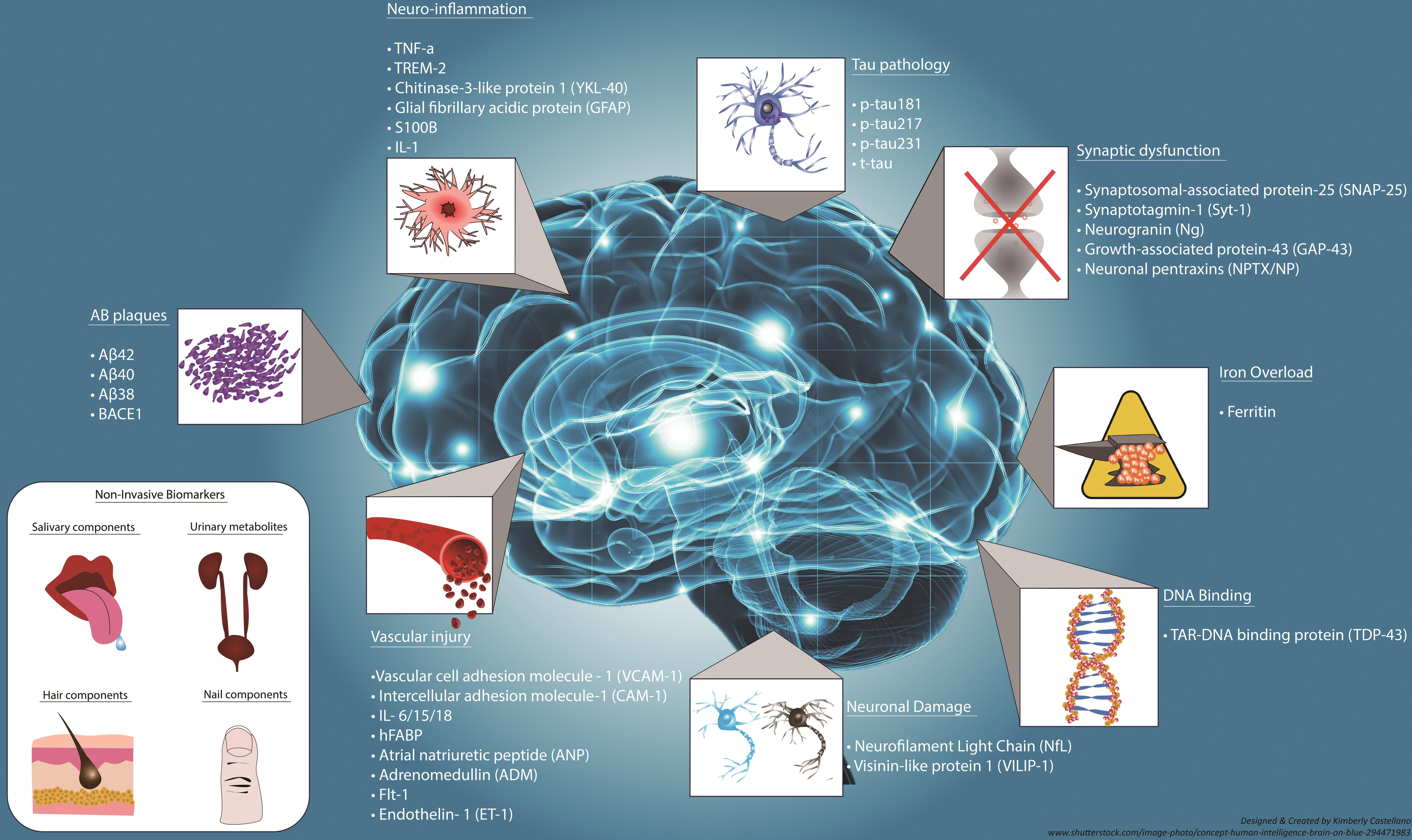
Biomarkers for Alzheimer’s: Early Detection and Diagnosis
The search for reliable biomarkers for Alzheimer’s disease has gained momentum in recent years, with research highlighting various potential indicators of the disease’s progression. Biomarkers related to microglial activity, synaptic pruning, and overall brain inflammation are receiving special attention. These biomarkers can provide critical information on the presence of neurodegenerative processes long before the onset of severe symptoms, allowing for earlier intervention. Discoveries from Stevens’ lab reinforce the importance of understanding these biological signals and their role in ensuring timely diagnosis and treatment of Alzheimer’s.
Furthermore, leveraging advanced diagnostic tools and integrating these biomarkers into routine clinical practice could revolutionize Alzheimer’s care. As the medical community strives to combat the pending Alzheimer’s epidemic, which is expected to see cases double by 2050, timely identification of individuals at risk becomes crucial. The implementation of biomarker-driven diagnostics not only enhances our understanding of Alzheimer’s but also enables personalized treatment options based on individual patient profiles.
Advances in Alzheimer’s Treatments Through Neuroscience
Recent advances in neuroscience have paved the way for novel treatments targeting the underlying mechanisms of Alzheimer’s disease. Research on microglial cells has significantly altered the paradigm of treatment development, shifting focus towards immunotherapy strategies aimed at modulating brain inflammation. By understanding how these cells contribute to neurodegeneration, scientists like Beth Stevens aim to develop interventions that can slow or even reverse the impact of Alzheimer’s on cognitive function.
The potential for developing targeted therapies based on the interactions between microglial cells and various neurological pathways heralds a new era in Alzheimer’s treatment. With the groundwork laid by basic scientific research and ongoing clinical trials, we may soon see breakthroughs that transform the landscape of Alzheimer’s management, offering hope to the millions suffering from this challenging disease.
Exploring the Brain Immune System: Insights into Neurodegenerative Diseases
The brain’s immune system, primarily represented by microglial cells, plays an essential role in maintaining neurological health and integrity. As our understanding of neurodegenerative diseases expands, it becomes clear that this immune system is intricately involved in the pathways leading to conditions like Alzheimer’s and Huntington’s disease. Research efforts highlight the double-edged sword of microglial activity, recognizing their protective functions as well as their potential to contribute to neuroinflammation and cell death.
As researchers explore the complexities of the brain immune system, they are uncovering novel strategies to harness microglial functions for therapeutic purposes. By enhancing the protective roles of these cells while mitigating their harmful effects, scientists can pave the way for innovative treatments that target the root causes of neurodegenerative diseases. This integrative approach not only deepens our understanding of Alzheimer’s but also contributes to a broader strategy for combating various other brain disorders.
The Promise of Neurodegenerative Disease Research
The ongoing research into neurodegenerative diseases, particularly Alzheimer’s, promises to transform the landscape of neurological health and care. As scientists delve deeper into the roles of microglial cells, novel therapeutic avenues are emerging that not only focus on symptom management but aim to alter the disease’s trajectory. The combination of molecular biology, neuroimmunology, and cutting-edge technology enables researchers to explore previously uncharted territories of the human brain.
In light of alarming predictions regarding the prevalence of Alzheimer’s cases, continued investment in neurodegenerative disease research is imperative. By fostering collaboration between academia, industry, and healthcare providers, we can expedite the development of effective treatments and prevention strategies. This concerted effort could significantly reduce the burden of Alzheimer’s on individuals and society, ultimately leading to a brighter future for affected families.
Beth Stevens: A Leader in Alzheimer’s Research
Beth Stevens, an influential figure in Alzheimer’s research, has dedicated her career to understanding the intricate workings of microglial cells. Her transformative discoveries have not only shed light on the brain’s immune mechanisms but have also laid the groundwork for potential treatments targeting Alzheimer’s disease and other neurodegenerative disorders. Stevens’ work exemplifies the significance of curiosity-driven research and highlights how foundational science can lead to breakthroughs with real-world applications.
Stevens’ commitment to advancing our understanding of neurodegenerative diseases through rigorous scientific inquiry underscores the vital role that research plays in developing effective therapies. Her accolades, including recognition as a MacArthur ‘genius,’ reflect her contribution to the field while inspiring the next generation of neuroscientists to pursue pioneering investigations that could one day change the course of Alzheimer’s treatment.
Challenges and Opportunities in Alzheimer’s Research
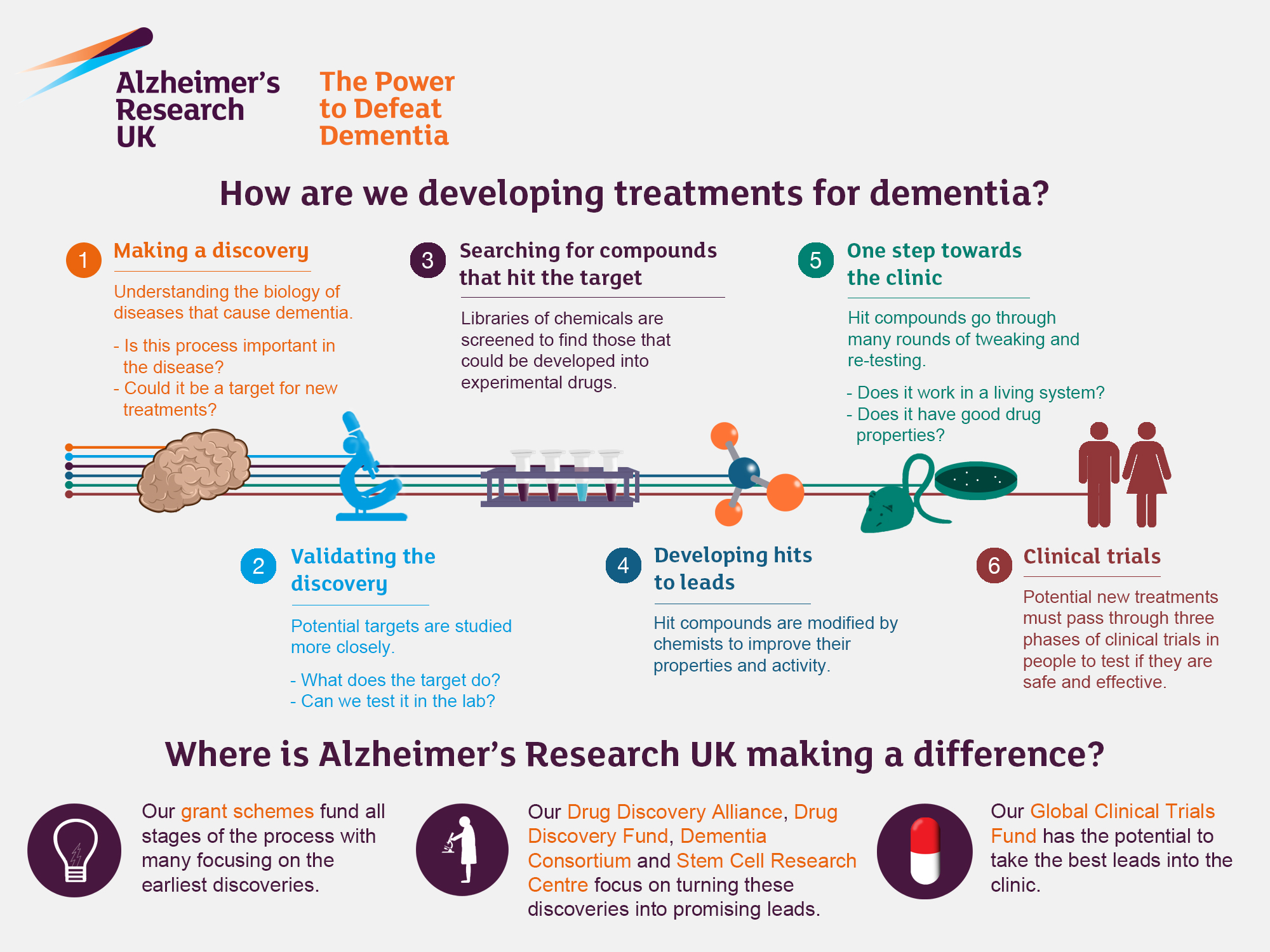
The path to effective Alzheimer’s treatments is fraught with challenges, ranging from complex pathophysiology to regulatory hurdles. Researchers confront difficulties in translating laboratory findings into clinical application, which often results in setbacks. However, these challenges simultaneously present opportunities for innovation. By embracing novel technologies, interdisciplinary collaboration, and a multi-faceted approach to neurodegenerative diseases, scientists can navigate these obstacles.
The collaboration between various fields, such as immunology and neurology, is crucial for addressing the multifaceted nature of Alzheimer’s. This integration of knowledge can lead to more holistic treatment strategies that target the disease’s underlying mechanisms rather than just its symptoms. The commitment to overcoming these challenges will be pivotal in making substantial progress in Alzheimer’s research and ultimately improving patient outcomes.
The Future of Alzheimer’s Disease Research
Looking ahead, the future of Alzheimer’s disease research is characterized by optimism and potential. With a wealth of information being generated through ongoing studies on microglial cells and other neurological pathways, researchers are poised to uncover deeper insights into the mechanisms of neurodegeneration. Emerging technologies, such as advanced imaging techniques and molecular profiling, are redefining how we understand Alzheimer’s pathology and facilitating the discovery of new therapeutic targets.
Moreover, as society becomes increasingly aware of the ramifications of an aging population, the prioritization of funding and resources for Alzheimer’s research will remain imperative. The commitment to advancing science in this field not only enhances our understanding but also holds the promise of developing interventions that can significantly alter the course of Alzheimer’s, providing hope to millions globally and improving quality of life.
Community Impact and Alzheimer’s Awareness
Raising awareness about Alzheimer’s disease plays a crucial role in fostering community support and enhancing research funding. Engaging the public in discussions about the importance of Alzheimer’s research helps demystify the disease, reducing stigma and promoting understanding. This awareness can lead to increased participation in clinical trials and support for advocacy efforts that push for more resources directed towards effective treatments and preventative strategies.
Community-driven initiatives are essential in providing resources for families affected by Alzheimer’s, as well as promoting educational programs that inform individuals about the signs and symptoms of the disease. By building a supportive environment, communities can play a vital role in helping those affected navigate the challenges posed by Alzheimer’s, while also advocating for greater scientific inquiry and improved care solutions.
Frequently Asked Questions
What role do microglial cells play in Alzheimer’s research?
Microglial cells are the brain’s immune system, patrolling for illness and injury. In Alzheimer’s research, their role has shifted from being merely protective to also understanding how aberrant pruning by these cells can contribute to neurodegenerative diseases like Alzheimer’s, thus providing insights for potential treatments.
How are neurodegenerative diseases linked to Alzheimer’s research?
Alzheimer’s research explores the mechanisms of neurodegenerative diseases, focusing on how factors like dysfunctional microglial cell activity can lead to conditions such as Alzheimer’s. By studying these links, scientists aim to uncover new biomarkers and treatments that can address the underlying causes of these diseases.
What is the significance of the brain immune system in Alzheimer’s research?
The brain immune system, primarily governed by microglial cells, plays a crucial role in Alzheimer’s research. It helps scientists understand disease progression and identify potential therapeutic targets that could halt or reverse the damaging processes associated with Alzheimer’s and other neurodegenerative conditions.
How are biomarkers for Alzheimer’s developed through current research?
Biomarkers for Alzheimer’s are being developed by investigating the roles of microglial cells and their activity in clearing damaged neurons. Research aims to find early indicators of Alzheimer’s disease by studying these cellular processes, paving the way for improved diagnosis and treatment interventions.
What advancements have been made in Alzheimer’s treatments based on recent research?
Recent Alzheimer’s research, particularly related to microglial functions and neurodegenerative pathways, has opened avenues for new treatments. This includes the potential for drugs that can modulate microglial activity, as well as strategies to identify biomarkers that can lead to earlier diagnosis and targeted therapies for Alzheimer’s.
| Key Point | Details |
|---|---|
| Role of Microglial Cells | Microglia act as the brain’s immune system, clearing damaged cells and pruning synapses. |
| Impact of Aberrant Pruning | Improper pruning by microglia can lead to neurodegenerative diseases like Alzheimer’s and Huntington’s. |
| Research Foundation | Stevens’ research is supported by significant federal funding, primarily from NIH. |
| Potential for Treatment | Findings could lead to new medicines and biomarkers for early detection of illnesses. |
| Alzheimer’s Statistics | The number of Alzheimer’s cases in the U.S. is expected to double by 2050, increasing care costs significantly. |
Summary
Alzheimer’s research is crucial in understanding and combating Alzheimer’s disease, as demonstrated by the groundbreaking work of Beth Stevens. Her studies on microglial cells reveal how these immune cells contribute to the pathology of neurodegenerative diseases through their pruning processes. By understanding the role of microglia, researchers can pave the way for innovative treatments and early detection methods, addressing the rising challenge posed by Alzheimer’s as the aging population grows. The potential impact of Stevens’ findings could change the landscape of Alzheimer’s care for millions and significantly reduce the future economic burden.